The Department of Radiology at the University of Wisconsin (UW) is engaged in cutting-edge research spanning the full spectrum of basic science, translational research, and clinical quality management in Computed Tomography (CT). The infrastructure includes state-of-the-art CT scanners, radiologists, physicists, dedicated research technologists, and a host of other research support personnel. We have many collaborative relationships with other departments throughout UWHealth and across the UW campus, including the Departments of Medical Physics and Biomedical Engineering.
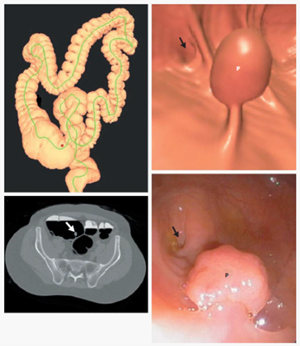
Pickhardt, Perry J., J. Richard Choi, Inku Hwang, James A. Butler, Michael L. Puckett, Hans A. Hildebrandt, Roy K. Wong, Pamela A. Nugent, Pauline A. Mysliwiec, and William R. Schindler. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults.external link New England Journal of Medicine 349, no. 23 (2003): 2191-2200.
Highlights of the CT research program include:
- The highly productive CT Colonography program is led by Dr. Perry Pickhard and Dr. David Kim. Dr. Pickhardt has produced over 250 publications in this area with multiple papers receiving over 1,000 citations.
- Work performed at the UW analyzing CT exams from outside institutions revealed that a major source of unnecessary exposure is due to unindicated multiphase scansexternal link. Dr. Christie Guite, the lead author on this study during her residency at UW Radiology, published the findings in the Journal of the American College of Radiology (JACR). JACR recognized her paper as one of the most outstanding papers they published in 2011.
- CT research at UW has totaled to more than 15 actively licensed patents and more than 30 issued patents over the last 10 years.
- To date, UW CT protocols have shipped to over 600 locations around the world as part of our research collaboration with GE Healthcare. Learn more about our CT Protocol work with GE.
Facility Overview
We have a variety of GE Healthcare CT scanners available for basic science and clinical translational research. Ranging from 32 to 256 slices, the scanners are state-of-the-art and feature the latest iterative dose-reducing reconstruction technologies as well as dual-energy imaging capabilities. Time is available for research on a dedicated research CT scanner located in the Wisconsin Institutes for Medical Research (WIMR) facility. The research scanner is a Revolution HD Discovery 750 system. This scanner is located adjacent to two MR systems (1.5T and 3T) and near an interventional bi-plane cone beam CT system and an operating suite, facilitating multi-modality research studies. Our facility has access to a micro CT unit and a cone beam CT unit for those interested in comparing these modalities for a specific imaging task.
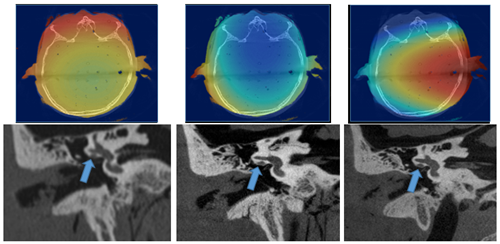
TP Szczykutowicz, S Schafer, K Royalty, SR Nace, and TA Kennedy.
Understanding the differences in radiation dose distribution between multi detector CT and C-arm CT for high contrast imagingexternal link
(Educational exhibit, presentation won cum laude honors). RSNA PHE-117 2014.